Did your pain start with an injury?
Yes, pain with injury is part of the process.
Did the pain remain beyond the time it was a useful signal?
In order to understand when an injury should stop hurting, let’s look at the steps your body went through to heal from an injury.
Step 1 in Healing
 Inflammation is the first step in body’s process of healing an injury.
Inflammation is the first step in body’s process of healing an injury.
The site of the injury swells, feels hot, looks red, is painful, and all these sensations combined cause a temporary loss of function of the injured part.
This is your body doing what it does best to heal the injury. The inflammatory process is necessary for healing to occur. It is predictable and will lead to healing.
How long it takes depends on the type of tissue injured and the severity of the injury. As well, your terrain is a factor: your healthy lifestyle habits, your stress level, your diet, evident in the health of your immune system. A tissue that is well supplied with blood, carrying the healing factors, will heal faster than one with less blood circulation.
In general, this step should last 3 days to a week.
Step 2
The second step of healing is repair, after the damaged tissue has been cleaned out and removed.
It can last from two to six weeks to repair or replace this damaged tissue.
The process in the body consists of laying down collagen fibers to rebuild the area. In essence, the area is regenerated by first laying down this scaffolding called collagen.
Step 3
When your body is done with producing collagen to repair the tissue, it moves on to remodeling. In this process the new tissue is modeled so that it is as much like what was lost as possible.
The tissue created during this process may be stiff and may not have found its proper direction, so movement is necessary to train the tissue to make it elastic and functional. This also strengthens the tissue so it can be “as good as new.”
This is the stage where we can get stuck.
As the pain is decreasing, we may want to resume movement of the area. But when we find that we are stiff and the area does not move like we are used to, then we may be reluctant to move it.
Unless the tissues are re-educated and shown what it is like to function properly in that part of the body, the stiffness will remain or even get worse. At this stage it is crucial to move in ways that retrain all the tissues involved in the area, whether it is joints, tendons, ligaments or muscles. Once movement returns to the level it was before the injury, the healing is considered complete.
These steps of healing are predictable and pain should be gone in three months.
Pain comes when healing is not complete
 If pain persists, inflammation has persisted and has become chronic. The acute inflammation of the first step was appropriate, but it is no longer appropriate at the end of healing.
If pain persists, inflammation has persisted and has become chronic. The acute inflammation of the first step was appropriate, but it is no longer appropriate at the end of healing.
There are many factors which can cause the inflammation to persist beyond the healing time. As we saw, the first was refusing to move when that was what the body was asking for in order to retrain the tissues.
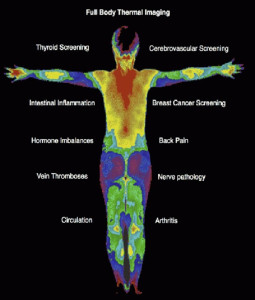
Most of the others have to do with your terrain – the environment in your body, mind and spirit that is the setting for healing to happen. As a reminder, terrain is influenced by nutrition, stress, ability to get oxygen to the tissues, and ability to remove waste from the tissues. The terrain may already be in a state of chronic inflammation from autoimmune disease, chronic infection or obesity.
When inflammation is chronic, pain will be there.
Pain comes when the brain decides
 The other possibility, whether there is chronic inflammation or the steps of healing were completed successfully, is that the brain had decided that to continue pain is in your best interest. Before you stop reading because I am blaming you for your pain, take a minute to follow this through. There is no blame, only understanding. First, let’s take a look at how we perceive pain.
The other possibility, whether there is chronic inflammation or the steps of healing were completed successfully, is that the brain had decided that to continue pain is in your best interest. Before you stop reading because I am blaming you for your pain, take a minute to follow this through. There is no blame, only understanding. First, let’s take a look at how we perceive pain.
There are many receptors in the body which, when stimulated, register different kinds of information. Some respond to pressure, others light touch, others heat, and others respond to damage or threat of damage. The latter are called nociceptors.
However, signals from nociceptor do not equal the sensation of pain. You have to make a decision whether the sensation that is detected is interpreted as pain. That is unconscious and happens in a millisecond. That decision is an emotional decision.
I’m sure you had an experience that showed you proof that it is not the particular sensation, but your emotional bias to the sensation that matters.
If it is the best day of your life, if you are getting married or there is some event that puts you in the best mood ever, and you stub your toe when you get out of bed, what happens? Does the pain of stubbing your toe ruin your day? I think not. It is a minor inconvenience and after hopping around and rubbing the toe, you go on with your most wonderful day. And the toe is not even painful.
If, on the other hand, you are feeling poor-me, down and out, feeling sorry for yourself because your life is not going like you wanted, and you stub your toe, what happens? That pain can be so overwhelming that you decide not to go on a wonderful hike planned the next day, and you might even have to check out whether you broke something. The instant the brain received the input from the nociceptor that there was damage in your toe, there was a decision whether it would impact your life or not. In this case, the stubbed toe was perceived as a threat to well-being, so was made a priority by making it painful.
Brain pathways adapt
Science has taught us a lot about the brain and pain.
We have found how the brain is capable of learning by acquiring new neural pathways and adapting. This is called neuroplasticity.
The brain is capable of adapting to new stimuli and reorganizing by creating new neural pathways, sprouting new connections to accommodate the new learning. The structure of the brain changes in order to adapt to new skills and it functions differently. For example, you can learn how to use a new device or a new language, no matter how old you are.
With persistent pain, it is precisely this neuroplasticity that is at the center of it.
Like we just learned, there is no nerve that transmits a signal of pain to the brain. It is the brain that takes into account all the signals it is getting and decides how to interpret it.
If you are consumed with fear, rage, or other strong negative emotions, that is taken into account. If an injury triggers memories and thoughts about them which are downward spiraling, that is also input. Your sensory organ signals are also taken into account. In addition, your brain cross-checks with stored beliefs, cultural norms and social expectations. If enough of these signals are perceived as a danger to you, then it will produce the sensation of pain.
All this happens in a millisecond! This method of producing pain is why pain can change from day to day and throughout the day depending on stress and fear levels. It also explains why pain can be very different from person to person with apparently the same injury.
Nervous system sensitivity
 There is one other factor which is important to how you perceive pain.
There is one other factor which is important to how you perceive pain.
What makes a difference in pain level is how sensitive your nervous system is. Chronic pain is associated with central sensitization of the nervous system.
This means that the nervous system is in a state of heightened sensitivity continuously. Conditions such as fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome and interstitial cystitis most likely have central sensitization happening. As well, may cases of lower back pain, chronic neck pain, injuries from a car accident, pain following surgery, and osteoarthritis most like are persistent due to central sensitization.
Central sensitization is characterized by two factors whose medical terms are allodynia and hyperalgesia.
The first characteristic is when sensations which are not normally painful, like gentle touch, is perceived as painful. The touch signal traveling through a highly sensitive nervous system is registered in the brain as uncomfortable, as pain. Through a normally sensitive nervous system, it would simply be perceived as touch.
The second characteristic is when a threatening stimulus is perceived as more painful than the threat actually is. For example, if someone accidently steps on your foot, it would normally produce an ache. However, with central sensitization the pain would be over the top.
Here are some clues that you have developed central sensitization:
- pain from an injury lasting beyond three months
- pain from an injury spreading beyond the site
- pain switching sides
- pain that is worse with stress
- pain getting increasingly worse
- small movements are painful
- pain is unpredictable
- pain that is linked with previous trauma
- pain that is worse with certain thoughts or feelings
Chronic Pain is different
 In the case of central sensitization, pain does not equal harm!
In the case of central sensitization, pain does not equal harm!
In acute situations, pain is a signal that you need to pay attention because something has been hurt.
When it has become chronic, pain is no longer a reliable signal that there is damage. It is a residual signaling due to inflammation, the brain using other negative signals to boost the sensation into being interpreted as pain or nervous system hypersensitivity.
If you have developed central sensitization, the good news is that the neuroplasticity of the brain can also desensitize the nervous system.
If you have involved other negative memories, thoughts, or emotions in creating the sensation of pain, you can cultivate awareness and detach those and redefine them. You can even dissolve the charge on those memories with mind/body techniques. The one I prefer and teach is Ascension-Meditation.
If there is inflammation, the terrain can be modified through diet, movement, mental and emotional state, and if desired biotherapeutic drainage like using the Unda numbers.
Heal Your Pain Now
 Physical therapist Dr. Joe Tatta has written about this extensively in his book Heal Your Pain Now. He details the three causes of chronic pain and shares how he works with clients to relieve them of their pain.
Physical therapist Dr. Joe Tatta has written about this extensively in his book Heal Your Pain Now. He details the three causes of chronic pain and shares how he works with clients to relieve them of their pain.
He starts with loads of useful information. There are helpful quizzes to help assess your kind and amount of pain. He offers chapters on solutions through diet, movement, and brain training.
Are you in this boat? Although I do not do all the modalities he mentions in his book, what I do does help retrain the brain and clear the terrain. I myself recovered from chronic pain from autoimmune arthritis.
What is your experience with recovering from chronic pain?